How to Get Pregnant with PCOS
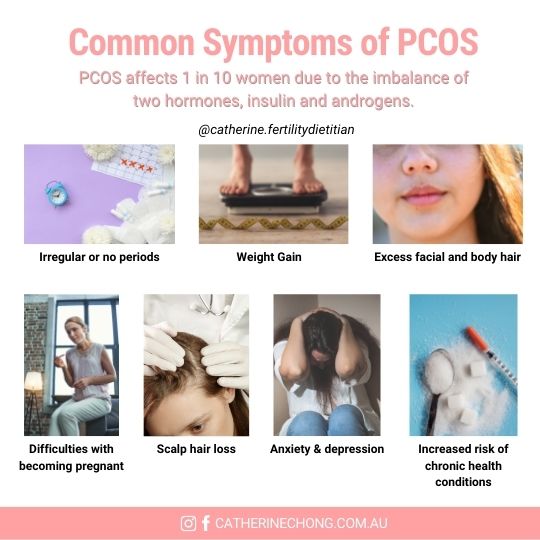
Polycystic Ovary Syndrome (PCOS) is a multifaceted hormonal disorder that affects women of reproductive age. Characterised by elevated levels of insulin and androgens (male-type hormones), PCOS often leads to symptoms such as irregular menstruation, difficulty conceiving, and metabolic disturbances.
In this guide, we’ll explore the key differences between PCOS and Polycystic Ovaries (PCO), updated diagnostic criteria for PCOS, and how PCOS affects fertility. Additionally, we’ll provide evidence-based diet and lifestyle tips to boost your chances of conception.
Understanding PCOS and Polycystic Ovaries (PCO)
It’s essential to differentiate between PCOS and Polycystic Ovaries (PCO), as they are distinct conditions:
PCOS:
- A syndrome involving multiple criteria, including hyperandrogenism, irregular ovulation, and polycystic ovaries on ultrasound. These criteria are outlined in the 2023 International Evidence-Based Guidelines.
PCO:
- Refers to the presence of multiple follicles on ultrasound without the accompanying hormonal imbalances or clinical symptoms associated with PCOS.
Understanding PCOS and Polycystic Ovaries (PCO)
It’s essential to differentiate between PCOS and Polycystic Ovaries (PCO), as they are distinct conditions:
PCOS:
- A syndrome involving multiple criteria, including hyperandrogenism, irregular ovulation, and polycystic ovaries on ultrasound. These criteria are outlined in the 2023 International Evidence-Based Guidelines.
PCO:
- Refers to the presence of multiple follicles on ultrasound without the accompanying hormonal imbalances or clinical symptoms associated with PCOS.
Updated Diagnostic Criteria for PCOS
The 2023 International Evidence-Based Guidelines share updated diagnostic criteria and advanced approaches for identifying PCOS:
Ultrasound Diagnosis of PCO:
- Polycystic ovaries are diagnosed using high-resolution transvaginal ultrasound, identifying ≥20 follicles per ovary or increased ovarian volume (≥10 mL).
- This update considers ultrasound technology advancements, which improve the detection of smaller follicles.
Criteria for Diagnosis of PCOS:
- Diagnosis requires two of the following: irregular ovulation, clinical/biochemical hyperandrogenism, or polycystic ovarian morphology on ultrasound.
- Exclusion of other endocrine disorders is mandatory for accurate diagnosis.
These evidence-based updates aim to improve diagnostic precision, ensuring timely and tailored interventions for women with PCOS. As a reminder, always consult your doctor if you have any concerns regarding your health.
How Does PCOS Affect Fertility?
PCOS disrupts normal ovulation through the interplay of elevated androgens and insulin resistance. This leads to multiple small ovarian follicles that fail to mature into dominant eggs. Additionally, hyperinsulinemia intensifies androgen production in the ovaries, further impairing ovulation and fertility.
How to Get Pregnant with PCOS: Updated Diet and Lifestyle Tips
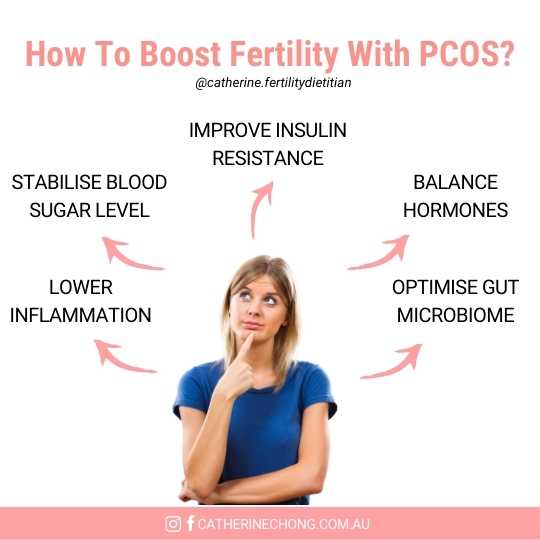
Achieving pregnancy with PCOS often requires a tailored approach that combines dietary, lifestyle, and sometimes medical interventions. Below are evidence-based strategies for improving fertility with PCOS.
1. Lower Carbohydrate Intake in Addition to Low-GI Diet
Women with PCOS often experience insulin resistance (IR), a condition that hinders ovulation and increases androgen levels. Research indicates that lowering overall carbohydrate intake and adopting a low-GI diet can improve insulin sensitivity, especially in individuals with severe IR.
A meta-analysis found that hypocaloric diets with reduced carbohydrates (<50% of total intake) significantly decreased IR. Improvements were even more pronounced in women with severe IR, highlighting the role of carbohydrate reduction in managing PCOS symptoms and improving fertility outcomes.
Additionally, low-GI (glycemic index) diets remain fundamental in managing PCOS. They help stabilise blood sugar levels and reduce insulin spikes, which is critical for improving ovulation and menstrual regularity. Studies demonstrate that low-GI diets significantly enhance ovulation rates and menstrual cycles in women with PCOS.
A systematic review and meta-analysis of randomised controlled trials demonstrated that low-GI diets improve key PCOS-related outcomes, including reduced insulin resistance, fasting insulin, total cholesterol, LDL cholesterol, triglycerides, waist circumference, and total testosterone. These benefits underscore the importance of incorporating low-GI diets into PCOS management to address both metabolic and reproductive health challenges.
Practical Tips:
- Keep carbohydrate consumption below 50% of daily calories, prioritising nutrient-dense, unprocessed, low-GI carbohydrates to stabilise blood sugar levels and maintain energy. Opt for whole grains like quinoa, farro, and rolled oats.
- Balance your meals with lean proteins and healthy fats to promote satiety, reduce blood sugar spikes, and support hormonal health.
- Gradually implement dietary changes under the guidance of a fertility dietitian to ensure your diet remains nutritionally adequate while targeting PCOS-related symptoms.
2. Support Gut Health: A Key Step in How to Get Pregnant with PCOS
Recent research underscores the vital role of gut microbiota in the pathogenesis of PCOS. Gut microbiota significantly influences lipid, glucose, and steroid hormone metabolism while regulating insulin synthesis and secretion. These mechanisms directly impact androgen levels, follicle development, and critical metabolic and reproductive health factors.
For individuals with PCOS trying to conceive, focusing on gut health can address underlying metabolic dysfunctions and improve fertility outcomes.
Practical Tips:
- To improve gut microbiota diversity, incorporate probiotic-rich foods such as yoghurt, kefir, and fermented vegetables.
- Increase your intake of prebiotic-rich foods like asparagus, onions, garlic, and barley to support healthy gut bacteria and improve hormonal balance.
By prioritising gut health, you may enhance your chances of getting pregnant with PCOS while supporting overall reproductive wellness. To learn more about fertility-boosting foods, read our previous blog here!
3. Consider Inositol Supplementation
Inositol supplementation, particularly in a 40:1 ratio of Myo-inositol to D-chiro-inositol, has been extensively studied for its positive effects on PCOS. It has been found to:
- Improve insulin sensitivity.
- Enhance ovulation and menstrual regularity.
- Support hormonal balance.
Research highlights the critical role of maintaining a proper Myo-inositol to D-chiro-inositol ratio for organ and tissue health, with imbalances linked to pathological conditions like PCOS. Ratios lower than 40:1 may reduce efficacy, while higher ratios, aligning with the natural follicular ratio of 100:1, show potential for improved outcomes. Further research is needed to evaluate the therapeutic impact of ratios exceeding 40:1 in PCOS management.
Always consult your healthcare provider before starting inositol or any other supplements, and ensure you follow the recommended dosages to maximise their benefits safely and effectively.
Bottom Line
- PCOS is a hormonal disorder that disrupts ovulation due to irregular cycles, elevated insulin, and androgens, leading to fertility challenges.
- Targeted nutrition, such as reducing carbohydrates and following a low-GI diet, improves insulin sensitivity and menstrual regularity.
- Supporting gut health with probiotic and prebiotic-rich foods enhances metabolic and reproductive health.
- Inositol supplements, particularly in a 40:1 ratio of Myo-inositol to D-chiro-inositol, further support hormonal balance and ovulation.
