How BPA Affects Your Fertility
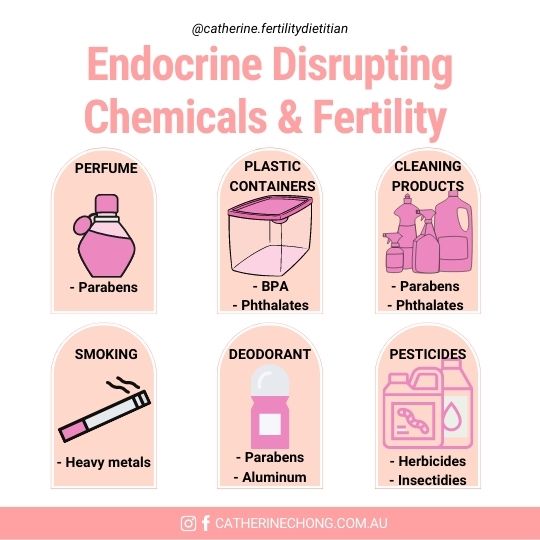
Endocrine-disrupting chemicals, particularly bisphenol A (BPA), have increasingly become a concern about their impact on fertility over the past 40 years. If you’re trying to conceive, understanding how environmental toxins like BPA impact your reproductive health is essential, as it has a significant impact on both male and female fertility.
This blog will explore the connection between BPA and fertility and offer proactive strategies to help reduce BPA exposure and protect your fertility journey.
What is BPA and Why Does it Matter for Fertility?
BPA has become a widely commercialised chemical that is integrated into various everyday products. It is a primary ingredient in hard polycarbonate plastics, thermal receipt paper, and epoxy resins, which are used as protective linings for food and beverage containers, industrial equipment, and piping. BPA is also commonly found in sealants used across industries, including construction and dentistry.
Tests commissioned by the Environmental Working Group (EWG) revealed that the amount of BPA present in thermal paper receipts is 250 to 1,000 times higher than the BPA level typically found in the lining of BPA-based food cans. This underscores the need for increased awareness and proactive measures to limit the day-to-day BPA exposure.
How BPA Disrupts Female Fertility
Research over the past two decades highlights a strong link between BPA exposure and female infertility. BPA disrupts the structure and function of critical reproductive organs, including the ovaries and uterus, by interfering with the hypothalamus-pituitary-ovarian axis. This hormonal disruption affects vital processes like the menstrual cycle, hormone secretion, oocyte development and embryo implantation, all essential for successful conception and pregnancy maintenance.
A recent study highlights the potential negative impact of BPA on reproductive outcomes in women undergoing in vitro fertilisation (IVF). Researchers analysed urinary BPA concentrations in 351 women at the Women’s Hospital School of Medicine at Zhejiang University. They evaluated their IVF outcomes, including oocyte retrieval, clinical pregnancy rates, and embryo implantation success. The findings revealed that higher urinary BPA levels were significantly associated with fewer retrieved oocytes and lower implantation and clinical pregnancy rates, even after adjusting for age, BMI, and other relevant factors.
These chemicals disrupt hormones, activate harmful receptors, induce oxidative stress, cause DNA damage, promote carcinogenesis, and trigger epigenetic changes, with intergenerational consequences. Epidemiological evidence links bisphenol exposure to reproductive system cancers, dysfunctions, miscarriages, and impaired pregnancy outcomes.
The Impact of BPA on Sperm Health
A recent systematic review and meta-analysis of 18 studies indicate that higher urinary BPA levels are negatively associated with sperm concentration and total sperm count. BPA exposure disrupts reproductive hormones, increasing sex hormone-binding globulin (SHBG) and estradiol (E2) levels while reducing biologically active androgen levels, essential for male fertility.
Although the link between BPA and clinically low sperm quality remains inconclusive, these findings highlight BPA’s potential to adversely impact male reproductive health and underscore the importance of minimising exposure.
Why BPS is Not a Safe Alternative to BPA
Although marketed as a safer choice, bisphenol S (BPS) exhibits similar, if not worse, endocrine-disrupting effects as BPA. Its ability to mimic hormones like estrogen, disrupt testosterone production, and interfere with developmental processes suggests that switching from BPA to BPS is not a solution but a lateral move to another harmful chemical.
Emerging research reveals a troubling connection between BPS exposure and numerous adverse outcomes related to fertility, pregnancy, impaired brain development and behaviour of future next generation. Another study analysing serum from infertile women undergoing fertility treatment found BPS levels were significantly higher than BPA, especially in women with recurrent implantation failure. These findings emphasise the need for caution with BPA alternatives in “BPA-free” products.
The growing evidence linking BPS to reproductive and developmental toxicity highlights the importance of reducing exposure to this chemical.
Practical Tips to Reduce BPA Exposure

While completely eliminating BPA from your environment may not be feasible, you can take practical steps to minimise your exposure:
- Switch to Safer Storage Options: Replace plastic food and beverage containers with glass or stainless steel alternatives.
- Choose Fresh or Frozen Produce: Minimise the consumption of canned foods when possible.
- Reduce Contact with Receipts: Limit handling of thermal paper receipts and choose digital receipts via email or text whenever available.
- Avoid Heating Plastics: Avoid microwaving food in plastic containers, as heat can cause BPA to leach into the food. Instead, use microwave-safe materials like glass or ceramic.
These small but impactful changes can significantly reduce your BPA exposure. To learn more about other holistic dietary approaches to optimise fertility, read our previous blog post here.
Bottom Line
- BPA is a widely used endocrine disruptor found in plastics, canned food linings, and receipts, with strong links to fertility issues in both men and women.
- BPA exposure disrupts hormone balance, reduces egg and sperm quality, and impacts reproductive health, such as implantation and pregnancy outcomes.
- You can start reducing exposure by using BPA-free containers, avoiding canned foods, limiting contact with receipts, and avoiding heating food in plastic.
