How to Get Pregnant with Endometriosis and Boost Your Fertility
Endometriosis is a chronic inflammatory condition affecting approximately 1 in 10 women during their reproductive years, making it a prevalent yet incurable disease that impacts millions worldwide.
This condition occurs when tissue similar to the uterine lining grows outside the uterus, leading to scarring and inflammation.
Women with endometriosis often experience elevated oestrogen levels, which are linked to the inflammation and pain associated with the condition. Common symptoms include pelvic and abdominal pain, bloating, heavy and painful periods, fatigue, painful intercourse, and, in some cases, infertility—which can contribute to up to 50% of infertility cases, depending on the stage of the disease.
In this blog post, we will share four nutritional strategies for boosting fertility and how to get pregnant with endometriosis.
How Does Endometriosis Affect Fertility and Pregnancy Success?
Endometriosis can negatively impact fertility by lowering egg quality, hormone balance, and ovarian health. The hormonal disruption caused by endometriosis, particularly an imbalance between oestrogen and progesterone, can impair egg maturation and increase the likelihood of genetic abnormalities.
Additionally, the inflammation triggered by endometriosis creates a hostile environment for egg development, leading to oxidative stress that can damage eggs. Over time, this inflammation may also harm the ovaries, reducing their ability to produce healthy, high-quality eggs, thus decreasing fertility and increasing the risk of miscarriage.
Fortunately, there is growing recognition that diet can play a key role in reducing the severity of endometriosis symptoms and enhancing fertility. Reducing inflammation through an endometriosis-friendly diet, which includes antioxidant-rich foods, can help counter oxidative stress. Moreover, incorporating specific foods that regulate estrogen production can further support fertility.
Top 4 Nutrition Strategies
The Role of Plant-Based Diet in Managing Endometriosis and Supporting Pregnancy
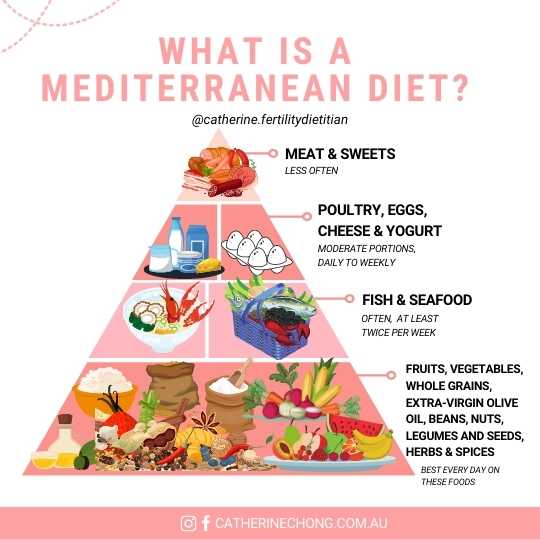
First, the Mediterranean diet, which emphasises plant-based foods, is considered one of the best dietary approaches to support endometriosis management.
Given the role of inflammation in endometriosis and how dietary changes can influence estrogen levels, plant-based diets have garnered clinical interest for their anti-inflammatory effects.
Extensive studies have shown that the quality of carbohydrates and certain types of fibre, specifically vegetable and cruciferous vegetable fibre, are scientifically linked to endometriosis diagnosis in premenopausal women, providing a solid basis for our dietary advice.
To learn more about including fertility-enhancing foods in your diet, read our previous blog post here.
2. Why Omega-3 Fatty Acids Are Essential For Endometriosis

Next, a higher intake of omega-3 fatty acids is linked to a 22% reduced risk of Endometriosis, while consuming trans-unsaturated fats is associated with a 48% increased risk.
Omega-3s, found in fatty fish like salmon, mackerel, and sardines, have strong anti-inflammatory properties and have been shown to reduce symptoms, including pain, in women with Endometriosis.
These healthy fats help lower inflammation and create a more fertile environment. In contrast, trans fats, commonly found in fried, baked, and highly processed foods, can increase inflammation.
Reducing your consumption of trans fats and opting for healthier fats like omega-3s can improve fertility and endometriosis symptoms.
3. The Importance of Vitamin D in Endometriosis
Vitamin D may help prevent and treat endometriosis. A 2020 meta-analysis found that low vitamin D levels were linked to a higher risk of endometriosis diagnosis and more severe symptoms.
In a randomised trial, women with endometriosis who took vitamin D supplements every two weeks for 12 weeks experienced a reduction in pelvic pain and decreases in high-sensitivity C-reactive protein, alongside an increase in total antioxidant capacity, suggesting its antioxidant and anti-inflammatory benefits.
If you’re considering starting a vitamin D supplement, it’s always best to consult your doctor and fertility dietitian before commencing the supplement.
4. Is a Gluten-Free Diet Essential for Endometriosis?
Research on whether a gluten-free diet improves endometriosis related pain and quality of life presents conflicting results.
One study found that a gluten-free diet may reduce endometriosis-related pain and enhance the quality of life for some women, as 75% of participants reported significant pain reduction after following the diet for 12 months. However, a critical narrative review concluded that while some women may benefit from eliminating gluten, there is currently no clear evidence of a causal link between a gluten-free diet and endometriosis symptom relief, and long-term adherence may lead to nutrient deficiencies.
Before making any changes, it’s essential to consult with a fertility dietitian to design a balanced, nutritious plan that supports both endometriosis management and fertility.
Bottom Line:
- A plant-based diet can help alleviate symptoms and improve reproductive health.
- Omega-3 fatty acids and vitamin D are powerful nutrients that have been shown to reduce inflammation and pain in women with endometriosis.
- Tailored nutritional plans in consultation with a fertility dietitian can effectively manage endometriosis while supporting fertility goals.
